Blood group, also known as blood type, is a category (type) of blood groups based on the presence and absence of blood group antigens in the surface (membrane) of the RBCs, and antibodies on the plasma.
- Several proteins, glycoproteins, glycolipids, and carbohydrates and their corresponding antibodies are studied to classify blood into specific blood groups.
- Since the classification of human blood into A, B, and C (which was later changed to O group) groups for the first time in 1901 by Karl Landsteiner, several other schemes are discovered to classify human blood into several blood groups. The International Society of Blood Transfusion (ISBT) has recognized 43 different blood group systems to classify human blood. However, the ABO system and Rh system of the blood group are considered the most important and are followed routinely for diagnostic, clinical, and forensic purposes.
Interesting Science Videos
What is Blood Grouping?
- The process of classifying blood into several blood groups based on the presence and absence of blood group antigens in the surface (membrane) of the RBCs and antibodies on the plasma is called blood grouping. Blood grouping is very important to prevent transfusion reactions and other disorders related to blood grouping antigens-antibodies reactions.
- In clinical and diagnostic labs, blood grouping is done using the antigen-antibody reaction method, and blood is mostly classified into ABO and Rh systems.
Common Blood Group Systems
Based on glycoproteins, lipoproteins, carbohydrates, and other proteins present several methods of typing the blood into different (43 different schemes) blood types have been discovered and recognized. However, all of them are not significant and studied.
Some of the common blood group systems recognized for their clinical relevance are listed below.
- The ABO blood group system: It is the oldest and the most important human blood group system which divides the blood into A, B, O, and AB types. (Details are described later below in a separate section.)
- The Rh system: It is another most important human blood group system which divides the blood into Rh+ and Rh- types. (Details are described later below in a separate section.)
- The MNSs blood group system: It is one of the oldest systems discovered in 1927. The classification system is based on the five most important antigens M, N, S, s, and U antigens; although 50 different antigens have been identified in this system. The blood group antigens are encoded by the Glycophorin A and Glycophorin B genes located on chromosome 4. The antibodies against these antigens are found in blood plasma but these are generally clinically insignificant.
- The P blood group system: It is a method of classifying human blood into different blood types based on the P-type carbohydrate antigens. It was identified in 1927 by Landsteiner and Levine. The P-type blood antigens are controlled by the B3GALNT1 and the A4GALT genes. There are 5 antigens in this system, namely P1, P2, P1K P2K, and P antigens, out of which, P, P1, and PK antigens are important and can cause transfusion reaction and erythroblastosis fetalis.
- The Lutheran blood group system: It is another system of blood group where the human blood is classified on the basis of the 19 Lutheran antigens present in the cell membrane of RBCs. These 19 antigens are encoded by variants of the BCAM gene and the system is based on the two co-dominant alleles, namely Lua and Lub. Phenotypically, the blood is classified into Lu (a+ b+), Lu (a- b-), Lu (a- b+), and Lu (a+ b-) blood types. This antigen and corresponding antibody system are rarely found to be associated with transfusion reaction and erythroblastosis fetalis.
- The Kell blood group system: It is the human blood group system based on the Kell antigens present encoded by the KEL gene. It was discovered in 1946. After the ABO and Rh systems, the Kell system is the third most important type of blood group system which can cause clinically significant transfusion reaction and erythroblastosis fetalis. In total, 25 different Kell antigens are known, but only 6 of them (K, k, Kpa, Kpb, Jsa, and Jsb) are clinically significant.
- The Lewis blood group system: It is the human blood group system based on the Lewis (Le) glycoprotein antigens encoded by the FUT3 (Lewis gene) gene and the FUT2 (Secretor) gene in chromosome 3. There are two major Le antigens Lea and Leb antigens with three major phenotypes: Le (a+ b-), Le (a- b+), and Le (a- b-).
- The Duffy blood group system: It is the human blood type first described in 1950, which is based on the Fy glycoprotein blood antigens present in the cell membrane of the RBCs. The Fy antigens are encoded by the DARC gene. Four Fy phenotypes viz. Fya+ b+, Fya+ b-, Fya- b+, and Fya- b- are major antigens of this system. These antigens and their corresponding antibodies are rarely associated with transfusion reactions and erythroblastosis fetalis.
- The Kidd blood group system: It is the human blood type based on the Kidd (Jk) glycoprotein antigens on the surface of the RBCs. This system was first identified in 1951. There are three major antigens named Jka, Jkb, and Jk3 encoded by the SLC14A1 gene found in chromosome 18. The Kidd antibodies can cause a severe hemolytic transfusion reaction.
- The Yt blood group system: Also known as the Cartwright blood group system, is a human blood type system based on the Yt antigens on the surface of RBCs. There are two major Yt antigens known, the Yta and Ytb antigens encoded by the ACHE gene. Antibodies of the Yt antigens are associated with delayed-type transfusion reactions.
- The Xg blood group system: It is a blood type based on the Xg protein antigens in the cell membrane of RBCs and corresponding antibodies on the plasma. It was first described in 1962. This system contains two major antigens; Xg(a) and CD99. The antigens of this system are encoded by the PBDX gene in the X chromosome. This blood type is not associated with any transfusion reaction.
- The Dombrock blood group system: It is a blood type based on the Do antigens in the cell membrane of RBCs and corresponding antibodies. It was first identified in 1965. Currently, five major antigens, Doa, Dob, Gya, Hy, and Joa, encoded by the ART4 gene are determinants of this blood type system. Severe transfusion reactions associated with Dombrock antigen-antibody reaction have been reported.
The ABO Blood Group System
- It is the most important and widely used human blood group system. It is the first blood group described by Austrian-born American biologist and physician Karl Landsteiner in 1901. Landsteiner in 1900 discovered that RBCs from one person’s blood agglutinate when mixed with the blood of another person. In the very next year, he classified blood into groups A, B, and C based on their agglutination properties. Later in 1910, Ludwik Hirszfeld and Emil Freiherr von Dungern named type C as type O. Thus, Landsteiner’s discovery led to the identification of agglutinogens A and B and agglutinins anti-A and anti-B leading to the classification of human blood into A, B, O, and AB types.
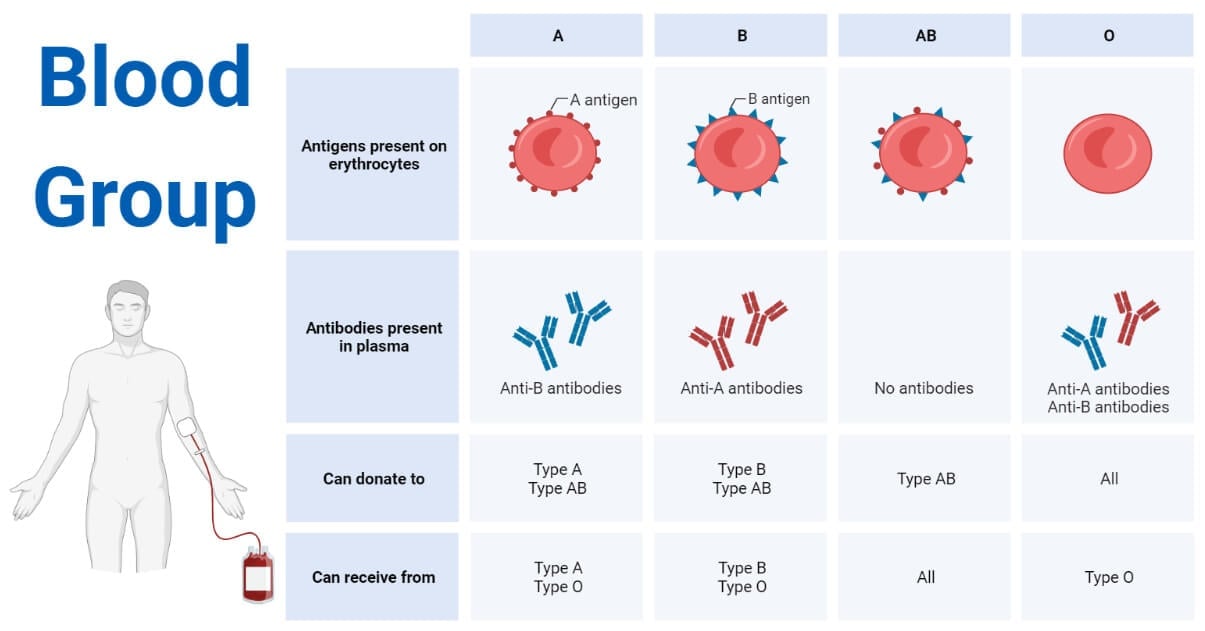
- The classification is based on the presence of either A antigen or B antigen or none of the antigens in the membrane of RBCs and the presence of anti-A or anti-B or both anti-A and anti-B antibodies on the blood plasma. The A and B antigens are glycoproteins found on the membrane of RBCs. These glycoproteins are encoded by the ABO gene.
- If the RBCs’ membrane contains A antigen and the plasma contains anti-B antibodies then the blood is classified as A-type blood.
- If the RBCs’ membrane contains B antigen and the plasma contains anti-A antibodies then the blood is classified as B-type blood.
- If the RBCs’ membrane contains both the A antigen and the B antigen and the plasma contains none of the antibodies then the blood is classified as AB-type blood.
- If the RBCs’ membrane contains none of the antigens and the plasma contains both the anti-A and the anti-B antibodies then the blood is classified as O-type blood.
- The ABO blood group system is under the regulation of the ABO gene containing three alleles, namely, i, IA, and IB. The IA and IB alleles are dominant over i, but they are co-dominant among each other. The expression of IA, IB, and i cause the expression of A, B, and O-type blood respectively. Gene with alleles IAIA or IAi phenotypically expresses type A blood. Similarly, individuals whose gene contains IBIB or IBi alleles, IAIB alleles, and ii alleles will have type B, type AB, and type O blood respectively.
- The A antigen and B antigen can violently react with anti-A and anti-B antibodies respectively leading to clumping of RBCs and immediate blood clot formation. This type of immune reaction causes a severe hemolytic reaction and there is a very high chance that a person will die if left untreated. Hence, ABO is considered one of the most important blood group systems, and human blood is always first classified according to the ABO type before transfusion or use for any medical or research purpose.
The Rh Blood Group System
- It is another most important human blood group system discovered by Karl Landsteiner and A.S. Weiner in 1940. They identified Rh antigens in the membrane of human RBCs and classified human blood into Rh +ve and Rh –ve types. (Rh is named after the Rhesus monkeys because their blood was used in determining the Rh antigens in human blood RBCs).
- Since the development of the Rh system 49 different Rh antigens (also called Rh factors) have been discovered. And among them, only five antigens, D, C, c, E, and e antigens, are clinically significant. Among them, Rh (D) antigen is highly immunogenic. It is the most studied and tested Rh antigen as it is associated with hemolytic reactions. These antigens are present in the transmembrane proteins, mainly in ion channels. These antigens are encoded by the RHD gene and the RHCE gene.
- The blood of a person having Rh (D) antigen in their RBCs is classified as Rh +ve type blood and the blood lacking Rh (D) antigens in their RBCs is classified as Rh –ve type blood. A person having Rh (D) antigens in their RBCs lacks the anti-D Rh antibodies in their blood plasma, but once the Rh (D) antigen is introduced into the bloodstream lacking Rh (D) antigen, the body synthesizes anti-D Rh antibodies.
- The anti-D, anti-C, anti-c, and anti-e antibodies can cause a hemolytic transfusion reaction. Among them, anti-D is the most potent and causes a fatal immune reaction, hence the human blood is always typed into Rh types before transfusion or before other purposes.
Prevalence/Frequency of ABO and Rh Blood Type
- Type O+ blood is the most prevalent type of blood and AB- is the least prevalent blood globally. Around 95% of people have Rh +ve type blood and only around 5% of people lack the Rh (D) antigen in their RBCs. Distribution of the blood types is varied among ethnic groups and people of different geographic locations. The global distribution of various blood types based on the ABO and Rh systems is summarized below.
| Blood Type (based on the ABO and the Rh system) | Percentage Prevalence (Globally) (approximately) |
| A+ | 31% |
| A- | 2.50% |
| B+ | 15% |
| B- | 1% |
| AB+ | 5% |
| AB- | 0.50% |
| O+ | 42% |
| O- | 3% |
Reference: World Population By Percentage of Blood Types – WorldAtlas
Method to Differentiate Human Blood into ABO and Rh types
- Human blood is routinely typed into ABO and Rh types for various medical purposes. The classification is based on the agglutination reaction principle. The agglutination reaction is an antigen-antibody reaction where an antigen reacts with its specific antibody and produces a visible clump under specific temperature and pH conditions. Human blood contains different blood group antigens in the membrane of RBCs and corresponding antibodies (agglutinins) in the plasma. When these antigens react with their corresponding agglutinins a visible clump is formed. This reaction is used to differentiate human blood into different ABO and Rh types in a lab.
- There are several methods available to group human blood like the slide method, tube method, microplate method, and automated method. The slide method is a widely used method and it is described below.
The slide method is the most popular and easy method of grouping blood.
Objective: To classify human blood into different ABO and Rh types
Requirements: Whole blood (mostly unclotted blood or fresh blood is preferred),
Glass slide, Wooden or plastic stick (toothpick), Dropper,
Blood Group reagents (anti-A antibody, anti-B antibody, anti-D antibody)
Procedures:
- Place 3 drops of blood, each in a separate glass slide or distantly in the same glass slide.
[If blood is in a tube you can use a dropper. You can also sterilize the fingertip of a person using spirit, then prick the finger using a sterile lancet and drops of blood in glass slides.]
- Place a drop of anti-A antibody (blue-colored antisera) over one drop of blood in the slide. Similarly, place a drop of anti-B antibody (yellow-colored antisera) over another drop of blood and finally a drop of anti-D antibody (colorless antisera) over a final drop of blood.
- Using a clean and separate stick, properly mix the antisera with the test blood drops.
- After about 2-5 minutes, look, with naked eyes, for the formation of visible clumps in the blood-antisera mixtures.
Observation and Conclusion:
- Look for the formation of visible clumps over the reaction mixtures.
- If a clump is formed in the mixture of blood and antisera-A, then the blood is type A.
- If a clump is formed in the mixture of blood and antisera-B, then the blood is type B.
- If a clump is formed in the mixture of blood and antisera-A and antisera-B both, then the blood is type AB.
- If a clump is not formed in the mixture of blood and both antisera-A and antisera-B, then the blood is type O.
- If a clump is formed in the mixture of blood and antisera-D, then the blood is Rh +ve type.
- If a clump is not formed in a mixture of blood and antisera-D, then the blood is Rh –ve type.
| Clumping on a Mixture of blood and | Blood Type | ||
| Anti-A | Anti-B | Anti-D | |
| √ | √ | A+ | |
| √ | A- | ||
| √ | √ | B+ | |
| √ | B- | ||
| √ | √ | √ | AB+ |
| √ | √ | AB- | |
| √ | O+ | ||
| O- | |||
Significances of Blood Grouping
- It helps to identify the blood type of an individual so that they can manage blood during medical needs.
- Blood grouping helps to prevent the hemolytic transfusion reaction during blood transfusion and/or organ transplantation.
- Blood grouping is also used in forensic science for the identification of persons.
- It is used in medicine and genetics to determine the blood type of a fetus and prevent erythroblastosis fetalis or other complications during pregnancy.
Blood Compatibility
- Blood compatibility means the ability of blood from different sources to co-exist and function properly without agglutination. Not all human blood are alike and the blood of one person may not be compatible with the blood of another person. Some blood group antigens and their corresponding agglutinins can violently react resulting in a severe hemolytic agglutination reaction which can be fatal. So, blood compatibility must be checked prior to blood or organ transplantation.
- Mainly ABO and Rh antigens and antibodies result in severe transfusion reactions, hence blood is primarily classified based on ABO and Rh system. The blood of the donor and the receiver is then checked for compatibility, also called cross-matching, prior to transfusion.
- The Rh +ve blood group is compatible with another Rh +ve blood only, and hence can’t be transfused to a person with Rh –ve blood type. Similarly, a person with A-type blood can’t receive blood from a person with B-type blood, and vice-versa. A person with O-type blood can only receive O-type blood. However, a person with AB-type blood can receive the blood of any type.
- The O -ve type blood is called the universal donor, as O -ve blood group can be donated to a person with any type of blood.
- The AB +ve type blood is called the universal acceptor as a person with AB +ve type blood can receive the blood of any type.
- The blood compatibility chart is summarized below:
| Blood Group of Possible Receiver | |||||||||
| Blood Group of Donor | A + | A – | B + | B – | AB + | AB – | O + | O – | |
| A + | √ | √ | |||||||
| A – | √ | √ | √ | √ | |||||
| B + | √ | √ | |||||||
| B – | √ | √ | √ | √ | |||||
| AB + | √ | ||||||||
| AB – | √ | √ | |||||||
| O + | √ | √ | √ | √ | |||||
| O – | √ | √ | √ | √ | √ | √ | √ | √ | |
Blood Transfusion Reaction
- Blood transfusion (BT) reaction is an immune reaction between the blood group antigens and their corresponding antibodies during or after the blood transfusion procedure. This type of reaction occurs due to blood incompatibility and other allergic or immunological conditions of the receiver. These reactions may be trivial allergic reactions to fatal type immune reactions. Mainly, ABO and Rh blood antigens and their corresponding antibodies are associated with blood transfusion reactions.
- The BT reactions are of two types; acute transfusion reaction and delayed transfusion reaction.
- The acute transfusion reaction is the BT reaction occurring during the blood transfusion process or within 24 hours of blood transfusion. It is primarily a result of ABO incompatibility. It may be of different clinical types based on clinical manifestation viz. mild allergic reaction, anaphylactic reaction, febrile non-hemolytic reaction, transfusion-associated circulatory overload, sepsis, acute hemolytic transfusion reaction, and transfusion-associated acute lung injury.
- The delayed transfusion reaction is the BT reaction that manifests usually after 24 – 48 hours of the blood transfusion. It is mainly associated with Rh incompatibility. Besides Rh antigens, Kidd antigens, Kell antigens, and Duffy antigens also cause the delayed type transfusion reaction. The delayed transfusion reaction is of two types based on its clinical manifestation; delayed hemolytic transfusion reaction and transfusion-associated graft-versus-host disease.
Erythroblastosis Fetalis
- Erythroblastosis fetalis is a hemolytic disorder of fetuses and neonates mainly due to Rh (D) incompatibility between the mother and the developing fetus inside her womb. It results in the destruction of the RBCs of the developing fetus and neonates causing hemolytic anemia in the fetus and the neonates.
- The fetal RBCs can freely move across the placenta and enter the maternal circulation during fetal development (pregnancy) and child delivery. If the fetus has Rh +ve blood and the mother has Rh –ve blood, then the Rh antigens in the child can trigger an immune reaction in the mother’s circulation. The infant’s blood may enter the mother’s circulation during delivery and also result in a similar immune reaction. Upon the introduction of the fetus’s Rh antigens, the mother’s body begins to synthesize Rh antibodies. The synthesized Rh antibodies will then attack the fetus’s RBCs and cause the destruction of the fetus’s RBCs leading to hemolytic anemia in the fetus.
- The Rh incompatibility between the mother and her first child may be mild and there is rarely serious harm to the fetus and newborns. However, if there is incompatibility during the second pregnancy also, then the developing infant has a higher chance to suffer from severe erythroblastosis (destruction of RBCs).
- Erythroblastosis fetalis can also occur due to ABO incompatibility, Kell incompatibility, Kidd incompatibility, Duffy incompatibility, and other blood antigen incompatibility.
- This condition can be diagnosed and prevented. Maternal blood typing and antibody screening, antibody level measurement in pregnant mother’s blood, cell-free fetal DNA screening, ultrasound of the fetus, a test of amniotic fluids, fetal middle cerebral blood flow measurement, fetal umbilical cord blood testing, RBC count in newborns, bilirubin test in infants, antibodies and Rh factor study in infants, etc. are followed in the medical lab for diagnosis of this condition.
- Treatment options include fetal blood transfusion, hydrating infants by IV fluids, intravenous immunoglobulin (IVIG) antibody therapy, etc. can be used to treat fetuses and infants suffering from this hemolytic disorder.
- Rh immunoglobulin (Rhig) also called RhoGAM is a preventive medication to prevent this disorder. This medication prevents from the development of Rh antibodies in the mother’s body.
References
- Mitra R, Mishra N, Rath GP. Blood groups systems. Indian J Anaesth. 2014 Sep;58(5):524-8. doi: 10.4103/0019-5049.144645. PMID: 25535412; PMCID: PMC4260296.
- Reid ME. MNS blood group system: a review. Immunohematology. 2009;25(3):95-101. PMID: 20406014.
- Judith Aeschlimann, Connie M. Westhoff, Chapter 28 – MNS and Duffy Blood Group Systems,Editor(s): Beth H. Shaz, Christopher D. Hillyer, Morayma Reyes Gil,Transfusion Medicine and Hemostasis (Third Edition),Elsevier,2019,Pages 163-167,ISBN 9780128137260,https://doi.org/10.1016/B978-0-12-813726-0.00028-3. (https://www.sciencedirect.com/science/article/pii/B9780128137260000283)
- Spitalnik PF, Spitalnik SL. The P blood group system: biochemical, serological, and clinical aspects. Transfus Med Rev. 1995 Apr;9(2):110-22. doi: 10.1016/s0887-7963(05)80050-1. PMID: 7795329.
- Daniels G. Lutheran. Immunohematology. 2009;25(4):152-9. PMID: 20406022.
- P blood group system | biology | Britannica
- Britannica, The Editors of Encyclopaedia. “Lutheran blood group system”. Encyclopedia Britannica, 15 Feb. 2019, https://www.britannica.com/science/Lutheran-blood-group-system. Accessed 13 January 2023.
- Rogers, Kara. “Dombrock blood group system”. Encyclopedia Britannica, 27 Oct. 2009, https://www.britannica.com/science/Dombrock-blood-group-system. Accessed 13 January 2023.
- Britannica, The Editors of Encyclopaedia. “Kell blood group system”. Encyclopedia Britannica, 15 Feb. 2019, https://www.britannica.com/science/Kell-blood-group-system. Accessed 13 January 2023.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. Chapter 8, The Kell blood group. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2270/
- Rogers, Kara. “Duffy blood group system”. Encyclopedia Britannica, 20 Feb. 2019, https://www.britannica.com/science/Duffy-blood-group-system. Accessed 13 January 2023.
- Britannica, The Editors of Encyclopaedia. “Xg blood group system”. Encyclopedia Britannica, 28 Oct. 2020, https://www.britannica.com/science/Xg-blood-group-system. Accessed 13 January 2023.
- Johnson NC. XG: the forgotten blood group system. Immunohematology. 2011;27(2):68-71. PMID: 22356523.
- Britannica, The Editors of Encyclopaedia. “Lewis blood group system”. Encyclopedia Britannica, 15 Feb. 2019, https://www.britannica.com/science/Lewis-blood-group-system. Accessed 13 January 2023.
- HUBINONT PO. Lewis blood-group system. Nature. 1949 Feb 12;163(4137):254. doi: 10.1038/163254b0. PMID: 18109172.
- Kidd blood group system | physiology | Britannica
- Lawicki S, Covin RB, Powers AA. The Kidd (JK) Blood Group System. Transfus Med Rev. 2017 Jul;31(3):165-172. doi: 10.1016/j.tmrv.2016.10.003. Epub 2016 Nov 9. PMID: 28065763.
- Rogers, Kara. “Yt blood group system”. Encyclopedia Britannica, 15 Feb. 2019, https://www.britannica.com/science/Yt-blood-group-system. Accessed 13 January 2023.
- ABO blood group system. (2023, January 1). In Wikipedia. https://en.wikipedia.org/wiki/ABO_blood_group_system
- Lawler, Sylvia Dorothy and Berkman, Eugene M.. “blood group”. Encyclopedia Britannica, 2 Nov. 2022, https://www.britannica.com/science/blood-group. Accessed 14 January 2023.
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. Chapter 7, The Rh blood group. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2269/
- Blood Types Explained – A, B, AB and O | Red Cross Blood Services
- Blood Types — Stanford Blood Center
- Blood groups – NHS (www.nhs.uk)
- Blood Groups | ABO Blood Group & Rh Blood Group Systems | BYJU’S (byjus.com)
- Blood groups – Better Health Channel
- BLOOD GROUPING – Histopathology.guru
- Blood Group Test Procedure, Interpretation, Result And More | Lab Tests Guide
- Determination of Blood Group | RBC | Blood Cells | Biology (biologydiscussion.com)
- Blood Group Testing- An experiment to determine the blood group (byjus.com)
- Blood Group Test Procedure and Results (noteshippo.com)
- Blood Groups: Definition, Concepts & Explanation – Embibe
- Blood Types — Stanford Blood Center
- Blood Compatibility Chart: Why Is Blood Compatibility Important? (hellodoctor.com.ph)
- Blood Type Compatibility | Memorial Blood Centers (mbc.org)
- Suddock JT, Crookston KP. Transfusion Reactions. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482202/
- Transfusion Reactions: Symptoms, Causes, & Complications (healthline.com)
- What Causes Transfusion Reaction Symptoms? (webmd.com)
- Blood transfusion reaction: Symptoms and treatment (medicalnewstoday.com)
