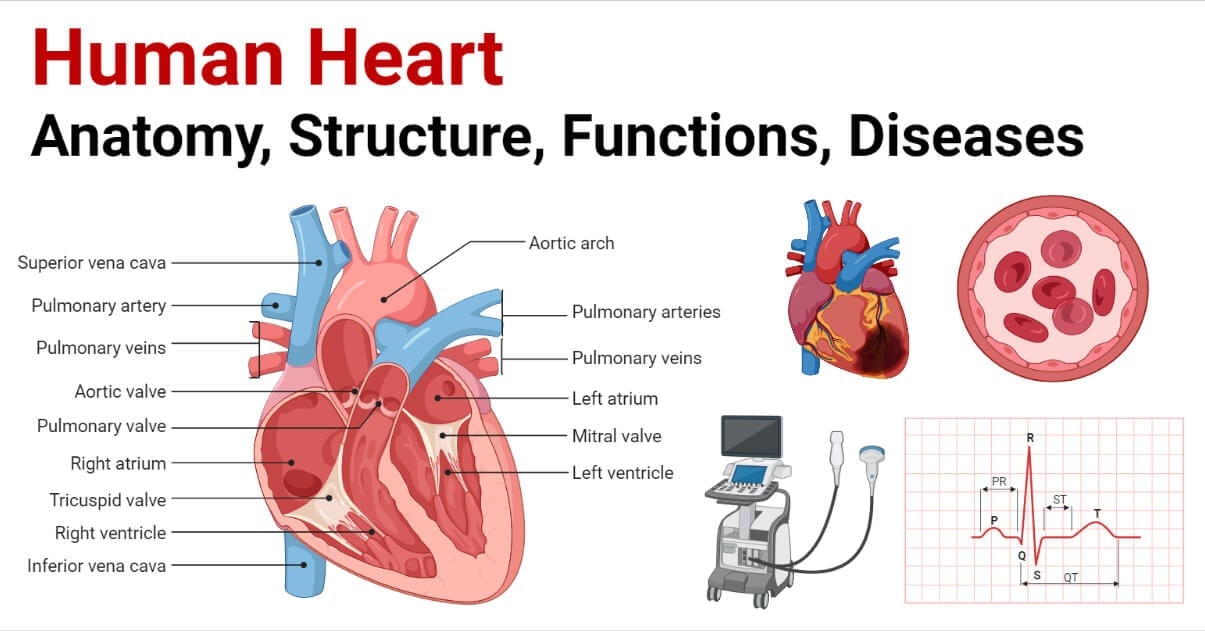
The heart is a hollow muscular pumping organ that generates pressure to circulate the blood through the blood vascular system under the influence of cardiac action potential.
In general terms, it is a pump that regularly propels blood throughout the body and collects it back for recirculation. It is the major organ of the blood circulation system (cardiovascular system).
In medicine, the heart is referred to as “cardio” like Kardia in Greek which means heart, and cardio/cardiac is used as a suffix to name any components or condition related to the heart. “Cardiology” is the study of the heart, and the “Cardiologist” is the doctor (or expert) of heart and heart-related conditions.
Interesting Science Videos
Location of Heart
- In humans, the heart is located mid-ventrally in the mediastinum of the thoracic cavity within a fluid-filled cavity called the pericardial cavity. Unlike the common belief that the heart lies on the left side of the chest, in reality, the heart lies in the center while its apex is slightly tilted towards the left side of the thoracic chamber.
- The heart is protected by the sternum and the ribs. The heart lies in between the sternum in front and the vertebral column behind and laterally it is placed in between the two lungs just above the diaphragm.
Morphology (Size) of Heart
- Externally, the heart is cone-shaped with an average dimension of (12- 13)×9×6 cm. It is slightly larger in males than in the female. The weight is about 300 grams (280 to 340) in males and only about 250 grams (230 to 280) in females. In an adult, the heart is approximately equal to the size of a clenched fist. The broader base lies upward slightly towards the right side part of the sternum, while the significant portion of the pointed apex lies slightly left to the sternum facing the diaphragm.
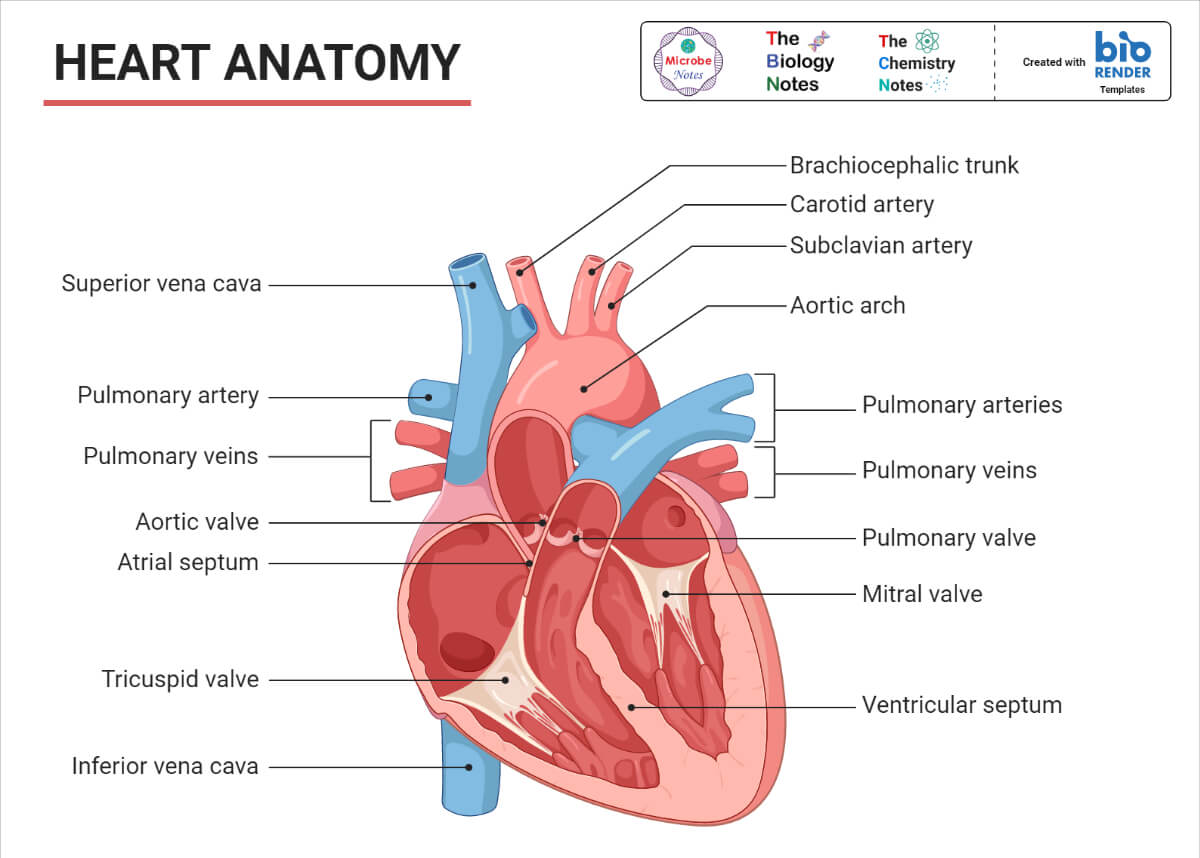
- The great vessels (aorta and vena cava) seem to be connected in the broader base part. The two major veins, the superior and the inferior vena cave enter the right atrium, and the aorta leaves from the left ventricle. Similarly, the pulmonary veins enter the left atrium, and the pulmonary artery leaves from the left ventricle.
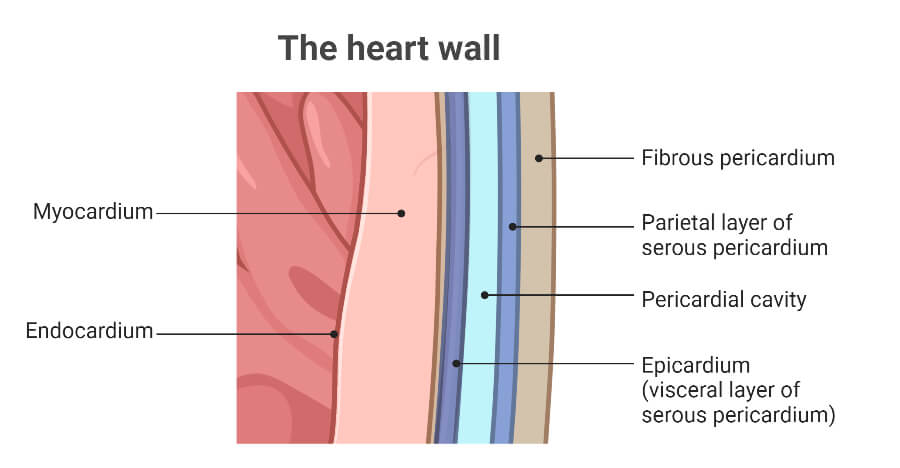
- The heart is surrounded externally by a protective fluid-filled fibrous membrane called the pericardium.
Pericardium
It is a double-layered tough membrane; the external layer is called the fibrous pericardium and the internal layer is called the serous pericardium.
The fibrous pericardium is the outer tough layer made of strong connective tissues. It forms a closed space within the mid-mediastinum to form the pericardial space. Posteriorly, it is fused with the central tendon layer of the diaphragm, anteriorly, it melds with the outer layer of the great vessels and completely seals the heart, and ventrally it is fused with the posterior end of the sternum. It provides mechanical protection to the heart.
The serous pericardium is the double-layered internal layer of the pericardium made up of mesothelium, a single layer of epithelium, which secrets the pericardial fluid. The outer layer internally lining the fibrous pericardium is called the parietal serous pericardium. There is a small cavity between the outer and the inner serous pericardium called the pericardial cavity, which is filled with the pericardial fluid.
This fluid provides lubrication that reduces the friction generated during the contraction and relaxation of the cardiac muscles, as well as protects the heart from mechanical shock. Forming the internal lining of the pericardial cavity, there is the inner layer of the serous pericardium called the visceral serous pericardium. It continues with the heart wall and is also called the epicardium.
Functions of Pericardium
- It protects the heart from mechanical shock, friction, and infection by serving as a tough physical barrier.
- It anchors and secures the heart in the mediastinum.
- It secrets the pericardial fluid, which helps to lubricate the heart during the heart contraction-relaxation process.
- It prevents the heart from over-expanding and over-filling and limits the heart’s motion by functioning as a tough, inflexible limiting membrane.
Heart Anatomy (Internal Structures)
1. Layers (Walls) of the Heart
The heart is a hollow muscular organ whose wall is anatomically divided into three distinct layers; epicardium, myocardium, and endocardium.
Epicardium
It is the outermost layer of the heart and the inner layer of the serous pericardium. It is composed of mesothelium tissues, fats, and connective tissues. It is fused with the adventitious layer of the major blood vessels. It serves multiple functions like protection from physical stress and friction, secretion of the pericardial fluid and factors for the proliferation of cardiomyocytes, signaling for heart development in the embryonic stage, and triggering the heart’s regeneration and healing response.
Myocardium
It is the middle layer of the heart wall made of specialized muscle cells called cardiomyocytes. It is the thickest muscular layer of the heart wall, also known as the heart muscle or the cardiac muscle. It is composed of striated, cardiac muscle cells, the cardiomyocytes, attached together by the intercalated discs and intertwined with the collagen fibers, cardiac fibroblasts, and extracellular matrix. This layer is supplied with coronary arteries and coronary veins for supplying the blood to the heart wall.
Myocardium serves by facilitating the rhythmic contraction and relaxation of the heart, providing a pathway for the conduction of the cardiac action potential, and forming the septum, which divides the heart into four chambers.
Endocardium
It is the thin innermost layer of the heart wall composed of three sub-layers the endothelium, the fibro-elastic tissues (collagen fibers, elastic tissues, and smooth muscles), and the connective subendocardial tissues. It internally lines all 4 heart chambers and the heart valves.
It provides a smooth surface for the free-flowing of blood inside the chambers and prevents the attachment of blood components in the heart wall. The connective subendocardial tissue layer contains the Purkinje fibers and hence helps in the transmission of cardiac impulses in the ventricles. Besides, the endocardium also provides covering and protection to the heart valves and regulates the ionic concentration of the cardiac cells.
2. Chambers of the Heart
The hollow heart of vertebrates is divided into different chambers by the heart muscles. These chambers serve to separate the pure (oxygenated) and impure (deoxygenated) blood and pump them accordingly for either purification or for the systemic supply. Humans (and other mammals) have four-chambered hearts i.e. our heart is internally divided into four compartments, two auricles (atria) and two ventricles, by the myocardial septum. The upper two chambers that receive blood are called the atria, and the two lower chambers from where blood is pumped out of the heart are called the ventricles.
The heart is divided into the right and the left side by the atrioventricular (AV) septum. The portion of the AV septum that separates the two atria is called the interatrial septum; whereas, the portion of the AV septum that separates the two ventricles is called the interventricular septum. The tricuspid valve and a short extension of the myocardium and AV septum separate the right atrium and the right ventricle. Similarly, the bicuspid valve and a short extension of the myocardium and the AV septum separated the left atria and the left ventricle.
The two chambers at the right part of the heart receive and pump out the impure blood. The right chambers of the heart receive and pump out pure blood.
Atria (Auricles)
Atria are the two upper chambers of the heart that receive blood from the two vena cava and the pulmonary veins. The two atria are named the right atrium and the left atrium based on their position. They are separated by the interatrial septum so that the blood of the two atria never comes in contact with each other. The atria are thin-walled chambers separated from the ventricles by the atrioventricular valves.
The right atrium is the upper right chamber of the heart where the superior and the inferior vena cava pour in the deoxygenated blood. Simply, it is the chamber for the collection of deoxygenated blood. It is located slightly right to the sternum and is structurally prominent with a slightly bulging and pyramidal shape. It receives blood from the vena cava and passes it to the right ventricle via the tricuspid valve.
The left atrium is the upper left chamber of the heart that receives pure (oxygenated) blood. Simply, it is the chamber that collects the oxygenated blood through the pulmonary veins. The aorta and pulmonary arteries are structurally located just above the left atrium. Structurally, it is slightly smaller than the right atrium and located left and slightly posterior to the right atrium.
Ventricles
Ventricles are the two lower chambers of the heart that receive blood from the atria and pump the blood out of the heart in either the systemic or pulmonary arterial system. Like atria, in a four-chambered heart system, the ventricles are also divided into the right ventricle and the left ventricle. Ventricles are larger than the atria and have a thicker muscular wall for mechanical pumping purposes. The two ventricles are separated by the interventricular septum and the components of the right and the left ventricles never come in contact.
The right ventricle is the lower right chamber that receives and pumps out the deoxygenated blood to the lungs for re-oxygenation. It is located behind the sternum and the terminal end is connected to the diaphragm. Externally, the atrioventricular (AV) groove marks the separating border of the right atrium and the right ventricle, whereas, the tricuspid valve marks the internal dividing border. During the atrial systole, the impure blood passes through the tricuspid valve and enters the right ventricle. During the ventricular systole, the blood is pumped through the pulmonary arteries.
The left ventricle is the terminal left chamber of the heart located slightly left of the sternum. It is the chamber with the thickest muscular wall. It receives the oxygenated blood from the left atrium during the atrial systole stage and pumps out the blood in the aorta (systemic arteries) during the ventricular systole stage. The AV groove marks the border of the left atrium and the left ventricle externally and the bicuspid valve separated them internally.
3. Heart Valves
The human heart is equipped with four major valves to prevent the backflow of blood in the heart chambers. The valves are the leaf-like structures (flaps) that maintain the unidirectional flow of blood inside the heart. These are highly organized connective tissue structures made of valve interstitial cells and organized extracellular matrix (composed of elastin, proteoglycans, and collagens) externally coated by endothelial cells and supported by papillary muscles and tendons.
These are activated by the blood pressure and open in one direction only when the blood pressure inside the respective heart chambers exceeds the threshold pressure required to open the valves. There is a total of 4 heart valves that are categorized into two groups; the atrioventricular valves and the semilunar valves.
Atrioventricular (AV) Valves
These are the heart valves present between the atria and ventricles that prevent checks from the backward flow of blood from the ventricles to the atria. The leaflets (cusps) of these valves are attached to the extensions of the ventricular heart walls by the subvalvular apparatus (structure made of chordae tendineae and papillary muscles). The pressure gradient developed during the atrial systole opens these valves and when they are closed just before the ventricular systole, they produce the first heart sound (S1) or the “Lub” sound of the heartbeat. There are two AV valves, namely; the tricuspid valve and the bicuspid valve.
The tricuspid valve is located between the right atrium and the right ventricle and prevents the flow of deoxygenated blood from the right ventricle to the right atrium. It contains three leaflets or the cusps, the anterior leaflet, the septal leaflet, and the posterior leaflet, hence got the name ‘tricuspid’.
The bicuspid valve, also known as the mitral valve, is located between the left atrium and the left ventricle and checks the flow of blood back to the left atrium from the left ventricle. It contains only two leaflets or the cusps, the aortic (anterior) leaflet and the posterior leaflet, hence got the name ‘bicuspid’.
Semilunar Valves
There are two semilunar valves present at the base of major arteries; the aorta and the main pulmonary artery (pulmonary trunk). They prevent the return of blood from the major arteries to the ventricles. These valves don’t have chordae tendineae and leaflet structures; instead, they have cusps that are self-supported within the arterial root. The pressure gradient developed during the ventricular systole opens these valves and when they are closed, they produce the second heart sound (S1) or the “Dub” sound of the heartbeat. There are two semilunar valves, namely; the aortic valve and the pulmonary valve.
The aortic valve is located at the base of the aorta and prevents the return of blood from the aorta to the left ventricle. These valves have three cusps; the left coronary cusp, the right coronary cusp, and the non-coronary cusp.
The pulmonary valve is located at the base of the pulmonary trunk. It is also tricuspid and prevents the return of blood from pulmonary arteries to the right ventricle.
4. Cardiac Impulse Conduction and Transmitting Channel
Humans have a myogenic heart i.e. the cardiac impulse which triggers the regular contraction and relaxation of the heart is generated by some specialized heart muscles (cardiomyocytes) but not by the neural impulses. These types of the heart are the features of vertebrates including humans. Whereas, some invertebrates like arthropods and annelids have a heart whose beating is initiated by neural impulses. Such types of hearts are called the neurogenic heart.
Cardiac Conduction System
The group of specialized cardiomyocytes that spontaneously generate the cardiac action potential (cardiac impulse) and transmit the generated action potential across the heart’s wall for the rhythmic beating of the heart is called the cardiac conduction system (or the heart’s conduction system or the electrical conduction system of the heart). The major components of the human heart conduction system include the sinoatrial node, atrioventricular node, Bundle of His, and Purkinje fibers.
Sinoatrial Node (SA Node)
The SA node is the center for the generation of the cardiac action potential at the rate of 60 to 100 times per minute. It is also called the natural Pacemaker of the heart and is composed of specialized cardiomyocytes called cardiac pacemaker cells. It is a small oval-shaped node of about 15 mm 3 mm 1 mm in dimension located at the right atrium below the superior vena cava.
Atrioventricular Node (AV Node)
The AV node is another mass of specialized cardiomyocytes that collects the cardiac impulses from the atria and relays them toward the ventricle for ventricular contraction. It is comparatively smaller than the SA node, measuring just about 5 mm 3 mm 1 mm in dimension, and is located near the ventricles at the end of the interatrial septum. It also generates cardiac impulses at a slower rate of 40 to 60 times per minute; hence it is also called the second pacemaker of the heart.
Bundle of His
It is a bundle of special cardiomyocytes that conducts the cardiac impulse from the AV node to the Purkinje Fibers. It arises from the end of the AV node and branches into the left and the right bundle branch and joins the major Purkinje fibers in the left and the right ventricle respectively.
Purkinje Fibers
These are small networks of specialized impulse-conducting cardiomyocytes that spreads the cardiac impulse across the ventricular wall. These cells are also capable of generating cardiac impulses but at a very slow rate of 20 to 40 times per minute if the pacemakers fail to function properly.
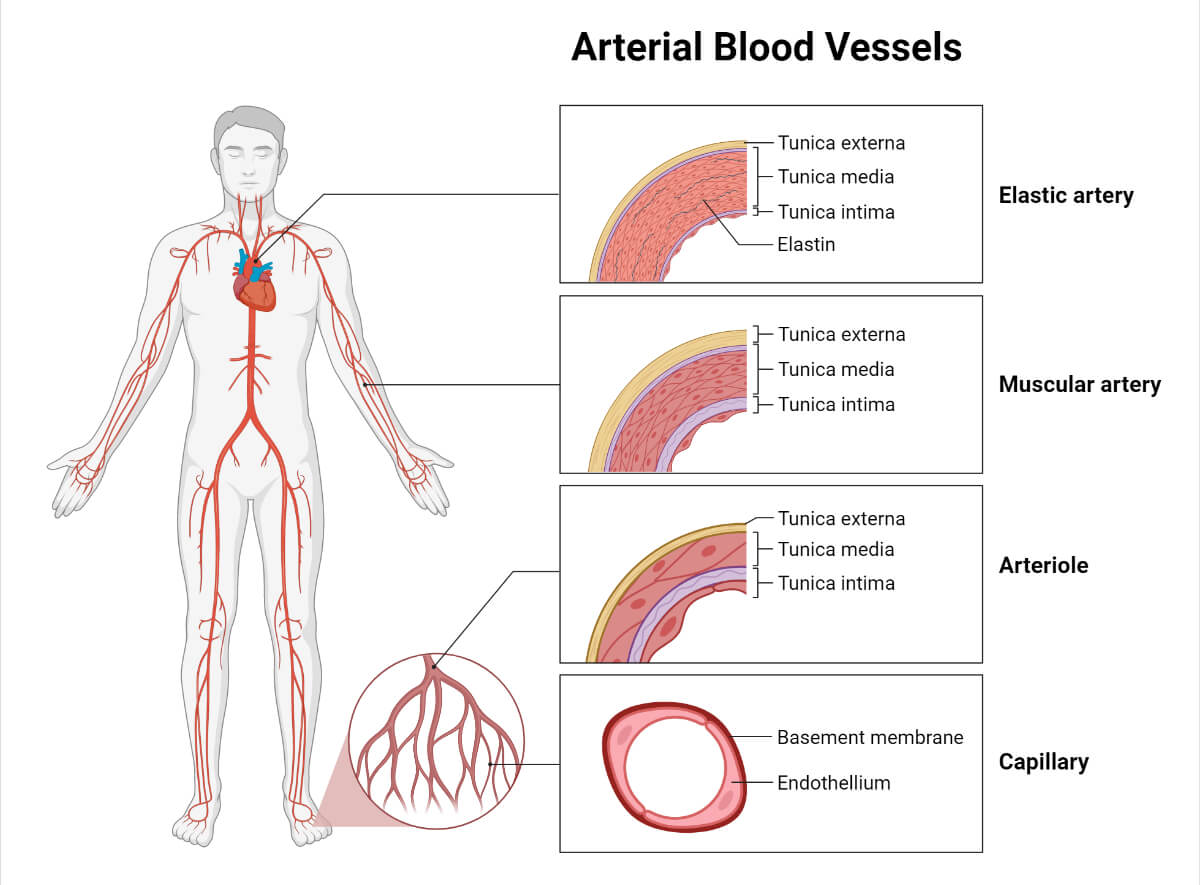
5. Coronary Vessels
Although the heart pumps blood to every part of the body and its chambers are regularly filled with blood, the heart muscles can’t absorb essential materials and excrete wastes in the blood within those chambers. Instead, the wall of the heart needs arteries and veins for blood circulation. These vessels supplying blood to the heart walls are called the coronary vessels and the circulation within the heart’s wall is called coronary circulation.
Coronary Arteries
These are the arteries that supply the oxygenated blood to the heart wall. They arise from the ascending arch of the aorta, within the cusp of the aortic valve. They arise as two major coronary arteries, the right main coronary artery (RCA) and the left main coronary artery (LCA) from within the right and the left cusps of the aortic valve respectively. These major arteries are further divided into major branches which again divide into smaller coronary arteries and coronary capillaries. The LCA supplies blood to the left ventricle and the left atrium. The LCA further divides into two major branches, the left anterior descending artery supplying the front side of the left side of the heart, and the circumflex artery supplying the outer and the back side of the heart. The RCA supplies blood to the right ventricle, the right atrium, and the AV and SA nodes. The RCA further divides into two major branches, the right marginal arteries, and the posterior descending artery.
Coronary Veins (Cardiac Veins)
Cardiac veins are the veins that drain the deoxygenated blood from the heart walls. There are seven major cardiac veins, (i) the great cardiac vein, (ii) the middle cardiac vein, (iii) the small cardiac vein, (iv) the posterior vein of the left ventricle, (v) the vein of Marshall, (vi) the anterior cardiac vein, and (v) the smallest cardiac vein (venae cordis minima). The first 5 major cardiac veins mentioned above merge together to form the coronary sinus which directly pours the blood into the right atrium. The anterior cardiac vein and the smallest vein independently pour into the right atrium.
6. Nerve Supply
The human heart is myogenic, however, the heartbeat and the heart rate are influenced by the nervous system. The human heart is supplied with a vagus nerve and the sympathetic cardiac nerve.
The cardiac vagus nerve is a nerve of the parasympathetic nervous system emerging from the brain stem and branching to connect the SA node and the AV node, which signals the reduction in the heart rate.
Similarly, the sympathetic cardiac nerve also arises from the brain stem, from the T1 to T4 thoracic ganglia. It branches and supply to the SA node, the AV node, the atria, and the ventricles. The sympathetic nerves promote the heart rate and the force of the heartbeat by releasing the noradrenalin neurotransmitter that tends to decrease the repolarization period.
Development (Cardiogenesis)
The heart is one of the earliest organs to develop during the human development period; it develops within about three weeks of fertilization. The process of development of the heart is called cardiogenesis.
The development of the heart is prominent from about 18 days of fertilization. The mesodermal tissue divides and begins the formation of the cardiogenic area within the 18-day-old embryo. In this cardiogenic area, two endocardial tubes are developed by the 20th day of fertilization. These tubes are forced into the embryonic thoracic cavity where they fuse forming the primitive heart (tubular heart) by day 22. Concurrently, other organs of the cardiovascular system also begin within the embryo.
The tubular heart contains the region of truncus arteriosus at the top followed by the truncus bulbus (bulbus cordis), primitive ventricle, the primitive atrium, and the sinus venosus downward.
From the 23rd day, cardiac looping, the process of folding the tubular heart in an “S” shape begins. The primitive truncus arteriosus metamorphose, develop, divide, and forms the aorta and the pulmonary trunk. The truncus bulbus and the primitive ventricle develop into the right and the left ventricle respectively. The primitive atrium develops into the anterior portion of the right and the left atrium. And, the sinus venosus metamorphose into the posterior portion of both atria. This process of chamber formation and the development of the septum is completed by the end of the 5th week (by the 35th day) of fertilization.
The AV valves are formed from the cavitation of the atrioventricular cushion and ventricular wall between the 5th and the 8th week, while the semilunar valves are formed from the cavitation of truncoconal ridge tissue between the 5th and the 9th week.
Physiology of Heart
1. Blood Flow and Cardiac Cycle
The heart is the key organ that conducts and regulates blood flow. The cardiac cycle is the process of regular contraction and relaxation of the heart chambers for conducting blood circulation. In humans, a cardiac cycle is completed in about 0.8 seconds. It is completed in two major stages; systole and diastole stage.
Systole is the stage where the chambers of the heart contract under the influence of cardiac impulses in order to expel blood. There are two systole stages; the atrial systole and the ventricular systole. Atrial systole is the process of contraction of the atrial wall to pump the blood of the atria into the ventricles. Ventricular systole is the stage where ventricular walls contract to pump the blood in the arteries expelling the blood out of the heart.
Similarly, diastole is the stage in the cardiac cycle, where the chambers of the heart relax allowing the blood to flow in. There are two diastole stages; the atrial diastole and the ventricular diastole. Atrial diastole is the stage where the pressure inside the atria decreases so that the blood from the major veins pours in allowing the blood to collect inside the atria. Also, the ventricular diastole is the stage where the blood from the atria enters the ventricles.
Blood flow cycle: The deoxygenated blood is collected by veins and poured into the right atrium via the superior and the inferior vena cava during the atrial diastole. From the right atrium, deoxygenated blood is passed to the right ventricle during ventricular diastole (or atrial systole). The blood is then pumped up to the lungs for purification via the pulmonary arteries during the ventricular systole stage. In the alveoli of the lungs gaseous exchange takes place making the blood oxygenated. The oxygenated blood is taken back to the left atrium via pulmonary veins during the atrial diastole. From the left atria, the oxygenated blood is passed to the left ventricle and is finally distributed all over the body through the systemic arteries during the ventricular diastole and the ventricular systole stage respectively.
2. Cardiac Conduction Pathway and Transmission Process
The cardiac impulse conducted by the SA node is relayed in an orderly fashion in a fixed channel, called the conduction pathway. The action potential is first build-up in the SA node by the pacemaker cells. The impulse is then transmitted over the intermodal tract and the Bachmann’s bundle across the right and the left atrial wall respectively. The impulse is transmitted at the speed of 0.07 meters per second in the intermodal tract and Bachmann’s bundle. However, the impulse is transmitted at a relatively low speed of about 0.05 m per second across the atrial wall.
Then the impulse is collected by the AV node. The AV node delays the impulse for about 0.09 seconds to let complete atrial depolarization and relay the impulse to the AV bundle where it travels at the speed of 0.05 meters per second.
The AV bundle interconnects the AV node and the Bundle of His and acts as the bridge to carry the action potential up to the Bundle of His. The Bundle of His and its branches have higher electrical conductivity and transmit the cardiac impulse at speed of 2 meters per second and transfer it to the Purkinje fibers.
Finally, the Purkinje fibers conduct the cardiac impulse all over the ventricular wall resulting in ventricular contraction. The Purkinje fibers have the highest conduction speed and relay the signal at the speed of 4 meters per second.
At the interventricular septum, the impulse transmits at speed of 0.16 meters per second, in the lateral ventricular wall the speed of cardiac impulse is about 0.2 meters per second, and in the lowermost ventricular wall, the speed of the cardiac impulse transmission is 0.18 meters per second.
Function of Heart
- Pumping of Blood: The heart regularly contracts and relaxes pumping the blood all over the body and again collecting it back for re-circulation.
- Generation and Transmission of Cardiac Impulses: The cardiac conduction system present in the heart generates the cardiac action potential and relays it all over the heart’s wall for myogenic regulation of the heartbeat.
- Maintaining Blood Pressure: The atrial systole and diastole generate the blood pressure and maintain the human blood pressure.
- The heart receives the deoxygenated blood and pumps the blood to the lungs for purification (re-oxygenation) purposes.
Did you KNOW?
On average, the human heart beats about 1,00,000 times each day and approximately more than 3 billion times in a lifetime (about 80 years), pumping about 6.8 liters of blood per minute.
Diseases Associated with the Heart
- Pericardial Effusion: Condition characterized by the accumulation of an excessive amount of fluid within the pericardial space.
- Pericarditis: Swelling/inflammation of the pericardium (often due to infections).
- Endocarditis: Swelling/inflammation of the endocardium (often due to bacterial infection).
- Stenosis: Narrowing of the blood vessels.
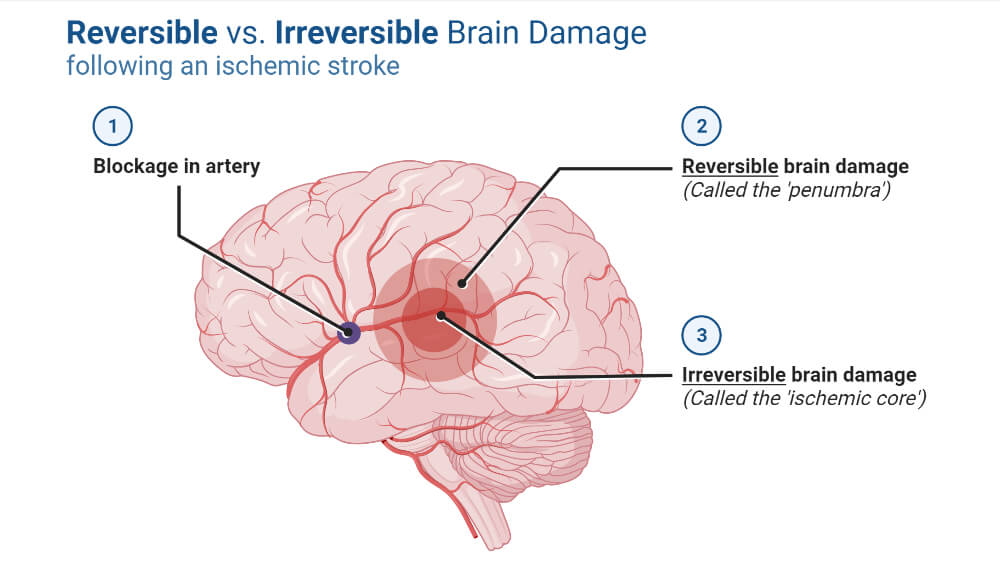
- Coronary Artery Disease (Ischemic Heart Disease): Condition characterized by deposition of the cholesterol (plaque formation) in the coronary arteries.
- Angina Pectoris: Chest pain due to insufficient blood supply in the heart muscles.
- Myocardial Infraction: Damage of the cardiac muscle due to lack of adequate blood supply.
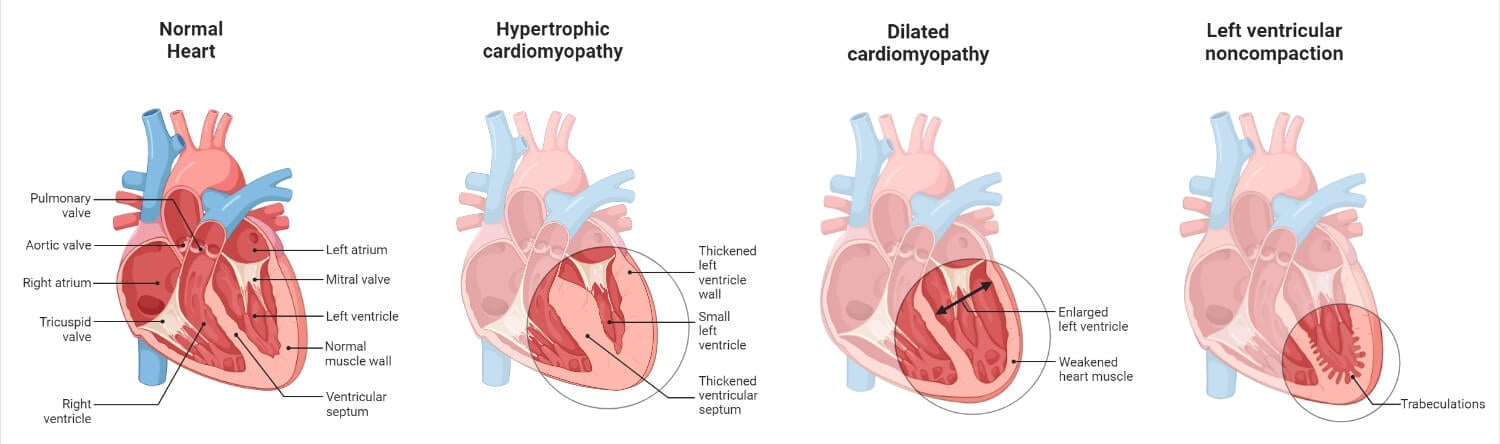
- Cardiomyopathy: Difficulty in the blood pumping process due to weakening of the cardiac muscle or decline in the ability of the cardiac muscle to generate sufficient pumping force.
- Cardiac Arrest: Sudden loss of heart function.
- Heart Valve Disease: Condition resulting in either one or more heart valves losing/declining in their function.
- Arrhythmia: Irregular heartbeat.
- Heart Murmur: Production of abnormal heart sound during a heartbeat.
- Mitral Valve Prolapse: Condition where the mitral valve is slightly pushed backward.
References
- Ross & Wilson Anatomy & Physiology in Health and Illness. 13th ed. Churchill Livingstone Elsevier. ISBN 978-0-7020-7276-5
- Keith L. Moore, Arthur F. Dalley, A. M. R. Agur. Clinically Oriented Anatomy. (2013) ISBN: 9781451119459 – Google Books
- Tortora, Gerard J.; Nielsen, Mark T. (2009). Principles of Human Anatomy (11th ed.) John Wiley & Sons. pp. 84–5. ISBN 978-0-471-78931-4.
- Hinton, R. B., & Yutzey, K. E. (2011). Heart Valve Structure and Function in Development and Disease. Annual review of physiology, 73, 29. https://doi.org/10.1146/annurev-physiol-012110-142145
- Chen PS, Joung B, Shinohara T, Das M, Chen Z, Lin SF. The initiation of the heart beat. Circ J. 2010 Feb;74(2):221-5. doi: 10.1253/circj.cj-09-0712. Epub 2009 Dec 18. PMID: 20019407.
- Kashou AH, Basit H, Chhabra L. Physiology, Sinoatrial Node. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459238/
- Wynn GJ, Noronha B, Burgess MI (2008). “Functional significance of the conus artery as a collateral to an occluded left anterior descending artery demonstrated by stress echocardiography”. International Journal of Cardiology. 140 (1): e14–e15. doi:10.1016/j.ijcard.2008.11.039. PMID 19108914
- Britannica, The Editors of Encyclopaedia. “heart”. Encyclopedia Britannica, 30 Nov. 2022, https://www.britannica.com/science/heart. Accessed 27 January 2023.
- Buijtendijk, F. J., & Barnett, P. (2020). Development of the human heart. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 184(1), 7-22. https://doi.org/10.1002/ajmg.c.31778
- Sylva M, van den Hoff MJ, Moorman AF. Development of the human heart. Am J Med Genet A. 2014 Jun;164A(6):1347-71. doi: 10.1002/ajmg.a.35896. Epub 2013 Apr 30. PMID: 23633400.
- How the Heart Works – How the Heart Beats | NHLBI, NIH
- Heart valves anatomy: Tricuspid-aortic-mitral-pulmonary | Kenhub
- The Pericardium – TeachMeAnatomy
- Pericardium: Function and Anatomy (clevelandclinic.org)
- Myocardium: definition, structure and function | Kenhub
- Epicardium: What Is It, Functions, and More | Osmosis
- Cardiac muscle. (2022, December 24). In Wikipedia. https://en.wikipedia.org/wiki/Cardiac_muscle
- Endocardium: What is it? Types of Layers, Functions and Associated Conditions – Scope Heal
- Endocardium: Function, Location, and Importance (verywellhealth.com)
- Layers of the heart: Epicardium, myocardium, endocardium | Kenhub
- Difference Between Myogenic and Neurogenic Heart | Compare the Difference Between Similar Terms
- Anatomy and Function of the Coronary Arteries | Johns Hopkins Medicine
- Coronary Arteries: Anatomy and Function (clevelandclinic.org)
- Human Heart: Diagram, Functions, & Importabt Facts – Embibe
- Human Heart – Anatomy and Functions | Location and Chambers (vedantu.com)
- CV Physiology | Normal and Abnormal Electrical Conduction
- What Are the Four Main Functions of the Heart? Common Heart Diseases (medicinenet.com)
- Human Heart – Anatomy and Functions | Location and Chambers (vedantu.com)
- Human heart: Anatomy, function & facts | Live Science
- How Many Times Does Your Heart Beat in a Lifetime? | Wonderopolis
- How the Heart Works – The Heart | NHLBI, NIH
- Human Heart (Anatomy): Diagram, Function, Chambers, Location in Body (webmd.com)
- Coronary Artery Disease | cdc.gov
- Human Heart – Anatomy, Functions and Facts about Heart (byjus.com)
- 16.1: Location of the Heart – Biology LibreTexts
- https://web.duke.edu/anatomy/embryology/embryoModules/cardiovascular/cardiovascular.html
- Heart embryology and congenital heart problems | Kenhub
- 19.5 Development of the Heart – Anatomy & Physiology (oregonstate.education)
- 17.5: Development of the Heart – Medicine LibreTexts
- Heart development. (2022, December 20). In Wikipedia. https://en.wikipedia.org/wiki/Heart_development
