Enterobacteriaceae is a family of Gram-negative, rod-shaped Gammaproteobacteria in the order Enterobacterales of the phylum Pseudomonatoda.
They are named so because they are primarily found in the small and large intestines of animals. They are also called “enteric bacteria” or “enterobacteria”.
They are cosmopolitan in habitat, and besides the intestine, they are also found in decaying vegetation and organic wastes, sewages, contaminated soil and water bodies, etc. Some of them are commensals, some are pathogenic, some are saprophytic, and some are endophytic.
A total of 68 genera including 355 species are currently proposed under the Enterobacteriaceae family. A large portion of them are normal flora of the human body, but some are responsible for mild to severe infections in humans. 26 genera are reported to be associated with human infection. Of these, E. coli, Klebsiella spp., Proteus spp., Shigella spp., Salmonella spp., Citrobacter spp., Enterobacter spp., Yersinia spp., Erwinia spp., Providencia spp., Hafnia spp., and Morganella spp. are the most common human pathogens in Enterobacteriaceae family.
Interesting Science Videos
Enterobacteriaceae Morphology
- Gram-negative bacilli of usually 1 to 5 μm (different species have different sizes)
- Predominantly motile (except species of Klebsiella and Shigella)
- Flagellated (mostly peritrichous flagella)
Enterobacteriaceae Biochemical Characteristics
- Facultative anaerobic
- Glucose fermentative
- Some ferment lactose while some can’t (based on these, they are grouped as lactose fermenters and lactose non-fermenters)
- Catalase positive
- Oxidase negative
- Nitrate reducing
- They have common antigens called “the enterobacterial common antigens” (ECA); the outer membrane antigen (O – antigen), the capsular antigen (K – antigen), and the flagellar antigen (H – antigen).
[Different species have different biochemical characteristics that are used for their identification]
Enterobacteriaceae Cultural Characteristics
Primary isolation media used for the isolation of Enterobacteria are:
MacConkey Agar (MAC)
Blood Agar (BA)
Nutrient Agar (NA)
Cysteine Lactose electrolyte deficient agar (CLED)
Brilliant Green Agar (BGA)
Thiosulfate citrate bile salt agar (TCBS)
Cetrimide Agar (CA)
Xylose Lysine Desoxycholate (XLD) Agar
Violet Red Bile Agar (VRBA)
Eosin Methylene Blue (EMB) Agar
Bile Esculin Agar (BEA)
Desoxycholate Citrate Agar (DCA)
For cultural characters, please visit: Enterobacteriaceae Cultural Characteristics – Microbe Notes
Enterobacteriaceae Clinical Manifestation
Enterobacteriaceae are responsible for a wide variety of diseases, acute as well as chronic, trivial as well as life-threatening. Some members like E. coli, Klebsiella spp., Enterobacter spp., Serratia ssp., Citrobacter spp., etc. are opportunistic pathogens; whereas, Salmonella spp., Shigella spp., Yersinia spp., some strains of E. coli, etc. are obligate pathogens. Different members are responsible for several clinical manifestations. The development of antibiotic resistance, especially to beta-lactam antibiotics, among Enterobacterales has increased the morbidity and mortality of infections caused by them. Some of the common diseases associated with Enterobacteriaceae are:
- Urinary Tract Infections
E. coli, Klebsiella pneumoniae, Proteus spp., Enterobacter spp., and Citrobacter spp. are the most common uropathogens. Mostly, they cause community-acquired UTIs, but hospital-acquired UTIs are also reported frequently.
- Respiratory Tract Infections
Klebsiella spp. (K. pneumoniae) is responsible for a large proportion of pneumoniae infections. In fact, it is the most common causative of pneumoniae after Streptococci. Proteus spp., Citrobacter spp., Providencia spp., Enterobacter spp., and Serratia spp. are also responsible for RTIs.
- Gastrointestinal Infections
Being enteric bacteria, many of the Enterobacterales are present inside the human intestine; however, some members and strains are highly pathogenic causing different types of gastrointestinal disorders.
Diarrhea is the most common GI tract infection caused by enteric bacteria. E. coli strains, Enterobacter spp., Salmonella spp., Shigella spp., Yersinia spp., Citrobacter spp., and Edwardsiella spp. are responsible for several forms of diarrhea, gastroenteritis, and enterocolitis.
Shigella spp. is responsible for dysentery, which accounts for the death of more than a million lives per year globally.
- Enteric Fever (Typhoid and Paratyphoid)
Salmonella Typhi and Paratyphi are causative agents of enteric fever.
- Soft Tissue and Skin Infection (Wound Infections)
E. coli, Klebsiella spp., and Citrobacter spp. are reported to be involved in wound infection. The prevalence of Enterobacterales in soft tissue infection is, however, very low.
- Others
Enterobacteriaceae are also associated with other infections like bloodstream infections (bacteremia and septicemia), neonatal meningitis, ulcers, folliculitis, plague, eye infections, etc.
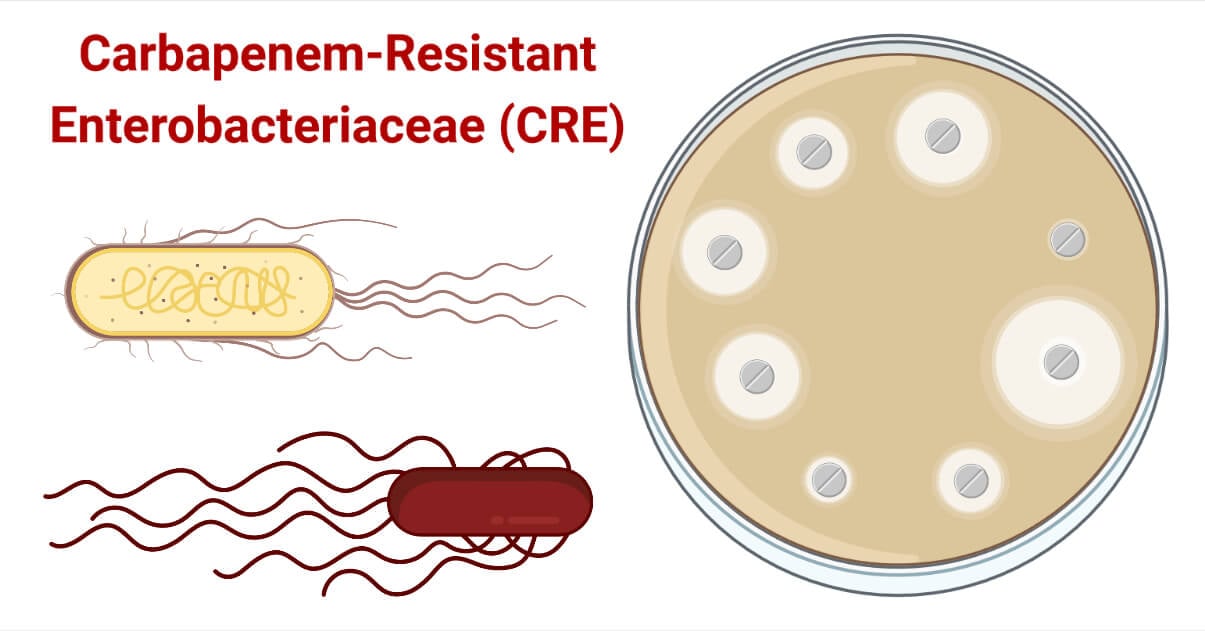
What are Carbapenem-Resistant Enterobacteriaceae (CRE)?
- Carbapenems are the broad spectrum Beta-lactam antibiotics having sulfur at the C-1 position and a double bond in between the C-2 and C-3 of the Beta-lactam ring with the side chains arranged in the trans position. They are used in the treatment of multidrug-resistant bacterial pathogens and hence, are called “the antibiotics of last resort”.
- The carbapenem antibiotics currently in use are “IMIPENEM”, “MEROPENEM”, “ERTAPENEM”, and “DORIPENEM”. Besides, Panipenem, Biapenem, and Tebipenem have also gained limited use, but they are still in the study phase.
- Several pathogenic bacteria have developed one or more mechanisms to escape the effect of carbapenems and are now completely resistant to carbapenems. Such organisms are called “Carbapenem-Resistant Organisms” (CROs). Some most serious carbapenem-resistant bacteria are:
- Carbapenem resistant Enterobacteriaceae (CRE)
[Carbapenem-resistant Klebsiella pneumoniae is the most important among them] - Carbapenem resistant Acinetobacter baumannii (CRAB)
- Carbapenem resistant Pseudomonas aeruginosa (CRPA)
- Beta-lactam antibiotics including Carbapenems are major antibiotics used against infections caused by Enterobacterales. However, many strains have developed resistance against one or more carbapenem antibiotics.
- Such Enterobacterales that have developed several mechanisms to protect themselves from the inhibitory or bactericidal action of carbapenems are Carbapenem-Resistant Enterobacteriaceae (CRE). Carbapenem resistance is seen mostly in healthcare-associated Enterobacteriaceae.
- Those enteric bacteria that confer resistance against carbapenems by producing carbapenemase enzymes are also called “Carbapenemase Producing Enterobacteriaceae” (CPE).
- The US Center for Disease Control and Prevention (CDC) defines CRE as any member of the Enterobacteriaceae family insensitive to at least one of the carbapenem antibiotics and has a minimum inhibitory concentration (MIC) value of 4 μg/ml for imipenem, meropenem, and doripenem, and MIC value of 2 μg/ml for ertapenem.
- CRE is labeled as “an urgent threat” by the US CDC in 2019 and “a priority 1 – critical pathogen” by the WHO since 2017.
- Carbapenem-resistant Klebsiella pneumoniae is the most important member of CRE.
- Infections caused by CRE are difficult to treat, need longer antibiotic courses and hospital stays, and have higher morbidity and mortality. Bloodstream infections and Pneumonia caused by CRE have a mortality of about 50%.
- The limited availability of antibiotics to treat has made CRPA a very serious pathogen.
History of Carbapenem-Resistant Enterobacteriaceae (CRE)
- The history of CRE is not long. In fact, carbapenems themselves were introduced recently in the late 1980s to tackle the infection caused by bacteria-producing extended-spectrum beta-lactamases (ESBL) enzymes.
- Unfortunately, many of the Enterobacteriaceae adapted themselves and developed several mechanisms to protect themselves from carbapenems. Soon after the introduction of carbapenems, in 1990, Carbapenem-Resistant Enterobacteriaceae (CRE) with the ability to produce Metallo-β–Lactamases enzymes capable of hydrolyzing carbapenems were reported from Japan.
- In 1996, the USA published a report on the carbapenem-resistant strain of K. pneumoniae. That strain of K. pneumoniae was declared endemic in New York City in the same year.
- By the early 2000s, several reports were published from different parts of the world mentioning CRE. It is 2009 when CRE is believed to spread across South Asia and all over the world.
Mechanisms of Resistance against Carbapenems by CRE
Enterobacteriaceae have evolved to cope with the effect of carbapenems in a very short period, just 10 years after the introduction of carbapenems in treatments. To achieve such resistance, they have developed three major mechanisms i.e. carbapenemase production, efflux overexpression, and porin modification.
1. Production of Carbapenemases
Carbapenemases are enzymes capable of hydrolyzing the – lactam ring of carbapenem antibiotics. Once hydrolyzed, they are useless and can’t inhibit the Penicillin-binding proteins (PBPs). Carbapenemase production is the primary mode of acquisition of resistance against carbapenems in Enterobacteriaceae. CPE is the most commonly isolated type of CRE. CRE are found to produce three major families of carbapenemases belonging to class A, class B, and class D Beta–lactamases as per Amber’s classification.
The carbapenemases that are produced by CPE are:
- Metallo-β-Lactamases (MBLs)
MBLs are the second most dominant carbapenemases produced by CRE across the world and the most dominant carbapenemases produced by CPE in the Asian region, mostly India and surrounding countries. New Delhi Metallo–β-Lactamase (NDM – 1) and Verona integrin-encoded Metallo-beta-lactamase (VIM) are the most common types of MBLs produced by CPE. IMP – 1 MBL is also reported, but its prevalence is very low and most cases are limited to China.
These MBLs enzymes are capable of hydrolyzing the entire Beta – lactams except monobactam.
- K. pneumoniae carbapenemase (KPC) β- lactamases
KPC Beta-lactamase production is the most commonly identified resistant mechanism in CRE. KPC – 2 and KPC – 3 are the predominant enzymes produced by CPE. US, South America, Europe, and East Asia are mostly infested with KPC Beta–lactamases producing CPE.
- Oxacillinase (OXA β- lactamases)
Oxacillinases are the third most dominant type of carbapenemase synthesized by CPE. OXA – 48, OXA – 181, and OXA – 232 are predominant Oxacillinase produced by Enterobacteriaceae. However, their major prevalence is seen in Mediterranean regions, Europe and North Africa. Distribution of carbapenemases in some most frequently isolated pathogenic Enterobacteriaceae:
| Enterobacteriaceae | KPC β-Lactamases (Class A) | MBL (Class B) | OXA β-Lactamases (Class D) |
| E. coli | √ | √ | √ |
| K. pneumoniae | √ | √ | √ |
| K. oxytoca | √ | √ | x |
| Proteus mirabilis | √ | √ | √ |
| Enterobacter spp. | √ | √ | x |
| Citrobacter freundii | √ | √ | x |
| Serratia marcescens | √ | √ | x |
| Morganella morganii | x | √ | x |
| Salmonella enterica | √ | x | x |
x = Not reported to produce the carbapenemase type
2. Modification in Membrane Permeability
Alteration of porin channels to block carbapenems from entering the cell is another mechanism of carbapenem resistance in Enterobacteriaceae. OmpK porin family is mostly altered in CRE.
3. Over Expression of Efflux Pumps
Over-expression of the efflux pumps is the second most prevalent carbapenem-resistant mechanism in CRE. The Resistance Nodulation Division (RND) efflux pumps are the most important type of efflux pump in CRE. The AcrAB – TolC RND efflux pump is the most dominant type in CRE.
Risk Factors for CRE Infections
- Elderly age
- Hospitalization and prolonged hospital stay
- Immunocompromised conditions
- Prolonged antibiotic treatments
- Recent surgery and open wounds
- Invasive medical devices like IV catheters
- Chronic diseases like Diabetic, cancer, and AIDS
Epidemiology of Carbapenem-resistant Enterobacteriaceae
- Since the first report of CRE in the mid-1990, CRE is now infecting people globally, mostly in hospital settings. Patient-to-patient transmission and the emergence of resistance within patients due to genetic alteration are the primary modes of acquisition. Besides, food supplies, water, soil, and career hosts (hospital staff) are also major sources of CRE dissemination.
- CRE was originally limited to healthcare facilities, but in several developing countries, especially in the Asian region, CRE is also reported in community settings.
- K. pneumoniae carbapenemase (KPC) β- lactamases producing CRE are endemic in the USA, South American countries (Brazil, Colombia, Argentina, Peru, Venezuela), Central American region, European regions (Italy, Greece), and China. Few reports of KPC-producing Enterobacteriaceae are released from the African region.
- Metallo-β-Lactamases (MBLs), especially New Delhi MBLs (NDM) producing Enterobacterales are mainly reported in Asia. It is declared endemic in South – Asian countries like India, Pakistan, Sri Lanka, and Bangladesh. Middle-East, China, and other Asian countries also have reported the isolation of MBLs producing CRE, but their prevalence is lower than in South Asia. NDM producers are also common in Romania, Poland, and Denmark. Verona integron-related Metallo-β-lactamase (VIM) producers are common in Spain, Hungary, and Italy. The NDM-1-producing Enterobacterales have been isolated in the US and Canada. Latin American countries and African countries are also publishing reports of CRE infections. MBL-mediated carbapenem resistance is an epidemic in African countries like Kenya, Nigeria, and South Africa. Other countries like Egypt, Morocco, Algeria, Tanzania, and Cameroon are also infected by NDM-producing Enterobacterales.
- Oxacillinase (OXA β- lactamases) producing Enterobacteriaceae, mainly OXA – 48 producers, are endemic in the Middle – East countries like Lebanon, Israel, Saudi Arab, Kuwait, and Oman, Turkey, Malta, and North African countries like Algeria, Morocco, Egypt, Libya, and Tunisia. They are also common in Mediterranean countries of Europe, South American countries (Argentina, Brazil, and Colombia), and Asian countries (India, China, Russia, Taiwan, and Thailand).
- Complete data on the incidence of CRE are not available, so, the exact distribution and epidemiological scenario can’t be expressed.
Identification of Carbapenem-resistant Enterobacteriaceae
Phenotypic identification methods based on the evaluation of MIC value and disc diffusion methods are commonly used. For the complete identification of mechanism and genetic data, molecular approaches are also available and are widely used for confirmation and research purposes.
A biochemical testing algorithm is the most commonly used for the identification of Enterobacteriaceae up to the species level.
Common biochemical tests used are:
Biochemical Algorithms for the Identification of Members of Enterobacteriaceae are
- IMViC Test (Indole, Methyl Red, Voges Proskauer, Citrate Utilization tests)
- Lactose Fermentation Test
- Sugar Utilization Tests
- Triple Sugar Iron (TSI) Test
- Motility Test
- Hydrogen sulfide (H2S) and Gas Production Test
- Urease Test
- Growth on KCN Medium
Biochemical test results for some of the most common Enterobacteriaceae are tabulated below.
| Bacteria | Indole | MR | VP | Citrate | Urease | H2S | Lactose fermentation | Motility | Growth on KCN |
| E. coli | +ve | +ve | – ve | -ve | -ve | -ve | +ve | +ve | -ve |
| Klebsiella | -ve | -ve | +ve | +ve | +ve | -ve | +ve | -ve | +ve |
| Proteus | -ve | +ve | -ve | +ve | +ve | +ve | -ve | +ve | +ve |
| Salmonella | -ve | +ve | -ve | -ve | -ve | +ve | -ve | +ve | -ve |
| Shigella | variable | +ve | -ve | -ve | -ve | -ve | -ve | -ve | -ve |
| Serratia | -ve | -ve | +ve | +ve | +ve | -ve | -ve | +ve | +ve |
| Citrobacter | -ve | +ve | -ve | +ve | variable | +ve | +ve | +ve | +ve |
| Yersinia | -ve | +ve | -ve | -ve | -ve | -ve | -ve | -ve | -ve |
| Enterobacter | -ve | -ve | +ve | +ve | -ve | -ve | +ve | +ve | +ve |
| Morganella | +ve | +ve | -ve | -ve | +ve | -ve | -ve | +ve | +ve |
| Providencia | +ve | +ve | -ve | +ve | -ve | -ve | -ve | +ve | +ve |
Confirmation of Carbapenem Resistance Enterobacteriaceae
A. Phenotypic Confirmation of CRE
Antimicrobial Sensitivity Testing and Calculation of Zone of Inhibition
Phenotypically, CRE can be confirmed by performing Antimicrobial Sensitivity Test using carbapenems. If the size of the zone of inhibition is less than recommended or in the level of resistance, then we can confirm the isolated Enterobacteriaceae to be CRE.
The breakpoint table for the interpretation of zone size for carbapenems against Enterobacteriaceae according to the CLSI standard is presented below.
| Zone Size (in mm) For: | Zone Size (in mm) For: | Zone Size (in mm) For: | |
| Carbapenem Antibiotics | Sensitive | Intermediate | Resistance |
| Doripenem (DOR 10 mcg) | ≥23 | 20 – 22 | ≤19 |
| Ertapenem (ETP 10 mcg) | ≥23 | 19 – 22 | ≤18 |
| Imipenem (IMP 10 mcg) | ≥23 | 20 – 22 | ≤19 |
| Meropenem (MRP 10 mcg) | ≥23 | 20 – 22 | ≤19 |
The breakpoint table for interpreting zone size for carbapenems against Enterobacteriaceae according to the EUCAST standard is presented below.
| Zone Size (in mm) For: | Zone Size (in mm) For: | Zone Size (in mm) For: | |
| Carbapenem Antibiotics | Sensitive | Intermediate | Resistance |
| Doripenem (DOR 10 mcg) | ≥22 | 17-21 | ≤16 |
| Ertapenem (ETP 10 mcg) | ≥25 | – | ≤25 |
| Imipenem (IMP 10 mcg) | ≥22 | 18-21 | ≤17 |
| Meropenem (MRP 10 mcg) | ≥22 | 17-21 | ≤16 |
Modified Hodge Test
Carbapenem Inactivation Method
EDTA Inhibition Test
Boronic Acid Inhibition Test
Carba NP Test
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS)
Chromogenic screening media are also under study but have found a limited use.
B. Molecular Confirmation of CRE
- Polymerase Chain Reaction (PCR)
PCR is the most widely used tool in laboratories for confirmation of CRE. PCR is used to identify carbapenemase-encoding genes and genes responsible for porin and efflux pump modification. - Duplex multiple cross displacement amplification combined with lateral flow biosensor (MCDA-LFB) method.
- Verigene Gram-negative blood culture assay (a nucleic acid non-amplification test based on the microarray principle which can detect blaCTX-M, blaKPC, blaNDM, blaVIM, blaIMP, and blaOXA genes in extracted nucleic acids)
- DNA Microarray is another commonly used method.
- BioFire Film Array Method (another automated multiplex PCR method mainly used for the identification of blaKPC genes)
- Xpert Carba-R method to detect blaKPC, blaNDM, blaVIM, blaIMP, and blaOXA-48
- Whole Genome Sequencing
Prospective Treatment Options for CRPA Infections
Treatment options for CRE are very limited and it is a very difficult task with a high chance of treatment failure. A precise treatment regimen is not established yet, but, combination therapy and high-dosage antibiotic administration are mostly practiced in healthcare facilities to treat CRE infections. Several pieces of research are going on for the development of appropriate treatment options for CRE infections.
Some of the currently available and in-use antibiotics are listed below:
- Polymyxins (Colistin and Polymyxin B)
They are the most widely used treatment option against CRE and are the therapeutic of choice. Colistins expel Magnesium ions (Mg+) and calcium ions (Ca++) from the lipopolysaccharide layer (LPS) disintegrating the cell membrane. They are effective against almost all the CRE and CPE.
- Tigecycline
It is used for the treatment of wound and soft tissue infections by CRE; however, it is not effective in bacteremia. It is active in that CRE with modified efflux pumps.
- Fosfomycin
High dosage fosfomycin in combination with carbapenem is effective against CRE. However, some Enterobacterales like K. pneumoniae, Enterobacter spp., and Serratia spp. are found to hydrolyze fosfomycin.
- Ceftolozane-tazobactam
- Ceftazidime-avibactam
It is used for CRE infections but is not effective against CPE-producing MBLs.
- Imipenem-cilastatin-relebactam
This combination therapy is effective against Enterobacteriaceae with modified efflux pumps and the ability to produce carbapenemases.
- Cefiderocol (limited use, in controlled clinical phase)
- Meropenem – Vaborbactam
It is effective against KPC, AmpC, and OXA Beta-lactamase-producing CPE, but is useless against MBLs producers.
- A single dose of an aminoglycoside
- Ciprofloxacin, Levofloxacin, Cotrimoxazole, and Nitrofurantoin (in those CRE that are sensitive to them) are also preferred in case of UTIs.
- Omadacycline (approved by FDA in case of community-acquired pneumonia and skin infection, but have limited availability)
- Ampicillin – Sublactam (Cefoperazone – Sulbactam)
- Sensitive carbapenem antibiotic (like extended–infusion meropenem in ertapenem-resistant Enterobacterales)
Future/Alternative Treatment Options Under Study
- Plazomycin and plazomycin in combination with ceftobiprole or daptomycin are found effective against MBLs producing CPE and other CRE.
- Cefederocol: it is a novel siderophore cephalosporin that has shown a good response against MBLs and KPC-producing CPE. It is a promising antibiotic that will be available globally in near future.
- Delafloxacin (Baxdale)
- Eravacycline
- Zidebactam
- Nacubactam
- Taniborbactam
- Fosamil – avibactam combination
- Nanoparticle therapy
- Phage therapy
- Engineered endolysins
- Vaccines
Prevention and Control Measures from CRE Infections and Spread
- Hand Hygiene: Proper cleaning of the hand with soap-water or antiseptics is recommended to prevent oneself from being infected. Especially, for hospital staff, proper hand hygiene practice before and after handling a patient is very important.
- Contact Precaution: Avoid physical contact with CRE patients without proper safety measures. Clinicians must practice proper contact precaution protocols.
- Education and Training for health professionals and common people.
- Isolation and Quarantine: Patients confirmed with CRE infection must be isolated in a separate room during their hospital stay. This way we can prevent the spread of CRE pathogens from patient to patient.
- Decolonization Protocols: Eliminating colonizing CRE from the human host or other reservoir is very important. Surfaces must be decontaminated.
- Surveillance to identify asymptomatic careers and reservoirs. Patients in ICUs, elderly patients, post-operative patients, hemato-oncology patients, ward patients with high colonization pressure, and long-term acute-care facilities (LTAC) need screening for colonization of CRE.
- Proper environmental sanitation.
- Sterilization and proper cleanliness practices in health care facilities and residential areas.
- Rational use of antibiotics
- Antimicrobial stewardship
- Proper and prompt laboratory diagnosis and adoption of the effective treatment regimen
- Continuous screening and surveillance for CRE pathogens.
References
- Janda, J. M., & Abbott, S. L. (2021). The Changing Face of the Family Enterobacteriaceae (Order: “Enterobacterales”): New Members, Taxonomic Issues, Geographic Expansion, and New Diseases and Disease Syndromes. Clinical microbiology reviews, 34(2), e00174-20. https://doi.org/10.1128/CMR.00174-20
- Human Pathogenic Enterobacteriaceae. C. Rock, M.S. Donnenberg, in Reference Module in Biomedical Sciences, 2014
- Patients | CRE | HAI | CDC
- Carbapenem-resistant enterobacteriaceae fact sheet | Children’s Health Queensland
- CRE | HAI | CDC
- Perez F, Bonomo RA. Carbapenem-resistant Enterobacteriaceae: global action required. Lancet Infect Dis. 2019 Jun;19(6):561-562. doi: 10.1016/S1473-3099(19)30210-5. Epub 2019 Apr 29. PMID: 31047851.
- Eser, Fatma. (2017). Carbapenem-resistant Enterobacteriaceae. Medical Journal of Islamic World Academy of Sciences. 25. 6-11. 10.5505/ias.2017.15045.
- Barber KE, Wagner JL, Larry RC, Stover KR. Frequency of and risk factors for carbapenem-resistant Enterobacteriaceae. J Med Microbiol. 2021 Feb;70(2):001286. doi: 10.1099/jmm.0.001286. PMID: 33263511; PMCID: PMC8131018.
- Richter SS, Marchaim D. Screening for carbapenem-resistant Enterobacteriaceae: Who, When, and How? Virulence. 2017 May 19;8(4):417-426. doi: 10.1080/21505594.2016.1255381. Epub 2016 Nov 4. PMID: 27813699; PMCID: PMC5477693.
- van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence. 2017 May 19;8(4):460-469. doi: 10.1080/21505594.2016.1222343. Epub 2016 Aug 11. PMID: 27593176; PMCID: PMC5477705.
- Duin, D. V. (2017). Carbapenem-resistant Enterobacteriaceae: What we know and what we need to know. Virulence, 8(4), 379-382. https://doi.org/10.1080/21505594.2017.1306621
- Han R, Shi Q, Wu S, Yin D, Peng M, Dong D, Zheng Y, Guo Y, Zhang R, Hu F; China Antimicrobial Surveillance Network (CHINET) Study Group. Dissemination of Carbapenemases (KPC, NDM, OXA-48, IMP, and VIM) Among Carbapenem-Resistant Enterobacteriaceae Isolated From Adult and Children Patients in China. Front Cell Infect Microbiol. 2020 Jul 3;10:314. doi: 10.3389/fcimb.2020.00314. PMID: 32719751; PMCID: PMC7347961.
- Suay, Beatriz & Pérez-Gracia, María-Teresa. (2019). Present and Future of Carbapenem-resistant Enterobacteriaceae (CRE) Infections. Antibiotics. 8. 122. 10.3390/antibiotics8030122.
- Iovleva, A., & Doi, Y. (2017). Carbapenem-Resistant Enterobacteriaceae. Clinics in laboratory medicine, 37(2), 303. https://doi.org/10.1016/j.cll.2017.01.005
- Yoo, H. (2018). The Infinity War: How to Cope with Carbapenem-resistant Enterobacteriaceae. Journal of Korean Medical Science, 33(40). https://doi.org/10.3346/jkms.2018.33.e255
- Trecarichi EM, Tumbarello M. Therapeutic options for carbapenem-resistant Enterobacteriaceae infections. Virulence. 2017 May 19;8(4):470-484. doi: 10.1080/21505594.2017.1292196. Epub 2017 Feb 8. PMID: 28276996; PMCID: PMC5477725.
- Alizadeh N, Rezaee MA, Kafil HS, Barhaghi MHS, Memar MY, Milani M, Hasani A, Ghotaslou R. Detection of carbapenem-resistant Enterobacteriaceae by chromogenic screening media. J Microbiol Methods. 2018 Oct;153:40-44. doi: 10.1016/j.mimet.2018.09.001. Epub 2018 Sep 4. PMID: 30189222.
- Tompkins, K., & Duin, D. V. (2021). Treatment for carbapenem-resistant Enterobacterales infections: Recent advances and future directions. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology, 40(10), 2053. https://doi.org/10.1007/s10096-021-04296-1
- Kelly AM, Mathema B, Larson EL. Carbapenem-resistant Enterobacteriaceae in the community: a scoping review. Int J Antimicrob Agents. 2017 Aug;50(2):127-134. doi: 10.1016/j.ijantimicag.2017.03.012. Epub 2017 Jun 21. PMID: 28647532; PMCID: PMC5726257.
- Akeda Y. Current situation of carbapenem-resistant Enterobacteriaceae and Acinetobacter in Japan and Southeast Asia. Microbiol Immunol. 2021 Jun;65(6):229-237. doi: 10.1111/1348-0421.12887. Epub 2021 May 19. PMID: 33913535.
- Potter RF, D’Souza AW, Dantas G. The rapid spread of carbapenem-resistant Enterobacteriaceae. Drug Resist Updat. 2016 Nov;29:30-46. doi: 10.1016/j.drup.2016.09.002. Epub 2016 Sep 19. PMID: 27912842; PMCID: PMC5140036.
- Lutgring JD. Carbapenem-resistant Enterobacteriaceae: An emerging bacterial threat. Semin Diagn Pathol. 2019 May;36(3):182-186. doi: 10.1053/j.semdp.2019.04.011. Epub 2019 Apr 17. PMID: 31056277.
- Durante-Mangoni E, Andini R, Zampino R. Management of carbapenem-resistant Enterobacteriaceae infections. Clin Microbiol Infect. 2019 Aug;25(8):943-950. doi: 10.1016/j.cmi.2019.04.013. Epub 2019 Apr 18. PMID: 31004767.
- Xu X, Qu F. [Progress in the diagnosis of carbapenem-resistant Enterobacteriaceae]. Sheng Wu Gong Cheng Xue Bao. 2018 Aug 25;34(8):1338-1345. Chinese. doi: 10.13345/j.cjb.170522. PMID: 30152219.
- Guidelines11FinalPrint (who.int)

please do add notes about Fermentation technology